Designed with WordPress
Category: gut health
-
by
-
More causative clues emerged when researchers began manipulating microbiomes to change phenotypes (observable traits, such as disease symptoms). Scientists would find a mouse model of fatty liver disease, for example, and then treat the mouse with antibiotics to erase its microbiome. If erasing the microbiome changed the liver disease or cured it, that suggested the microbiome was somehow involved.
— Read on magazine.hms.harvard.edu/articles/decoding-chemistry-microbiome -
Findings on Immune Dysfunction and Mental Health
Research has repeatedly demonstrated a strong connection between gut health and mental health. Immune dysfunction in the gut can lead to an imbalance in the gut microbiome, which is associated with a variety of psychiatric symptoms. Key findings include:
- Cytokine Production: The gut microbiome influences the production of cytokines—proteins that play critical roles in immune responses. Dysregulated cytokine levels have been linked to mood disorders such as depression and anxiety.
- Gut-Brain Axis: The gut and brain communicate bidirectionally through the gut-brain axis, a complex network involving the vagus nerve, immune system, and hormonal pathways. Alterations in gut health can signal the brain to exhibit changes in mood and behavior.
- Microbiome Composition: Studies have shown that individuals with psychiatric disorders often have distinct gut microbiome profiles compared to healthy individuals. A lack of specific beneficial bacteria has been associated with depression and anxiety disorders.
Justification for Probiotic and Prebiotic Treatments
Specific probiotic and prebiotic treatments can be beneficial in reducing psychiatric symptoms for several reasons:
- Restoration of Balance: Probiotics can help restore a healthy gut microbiome balance, potentially alleviating symptoms of anxiety and depression. For instance, Lactobacillus and Bifidobacterium strains have shown promise in reducing depressive symptoms in clinical trials.
- Enhancement of Gut Integrity: Prebiotics, which are dietary fibers that feed beneficial gut bacteria, can strengthen gut barrier function. A more robust gut barrier may reduce systemic inflammation and, in turn, positively influence mental health.
- Neurotransmitter Production: Certain probiotics can stimulate the production of neurotransmitters such as serotonin, the “feel-good” hormone, which is primarily synthesized in the gut. This can lead to improvements in mood and cognition.
Implications of Microbiome Diversity on Psychiatric Disorders
Diversity within the gut microbiome is crucial for overall health, including mental well-being. Low microbial diversity is often linked with psychiatric disorders. Implications include:
- Vulnerability to Stress: A less diverse microbiome may lead to increased vulnerability to stress and mental health disorders, as it may impair the body’s ability to respond to environmental challenges.
- Personalized Treatment: Understanding the specific microbial profiles associated with different psychiatric disorders can guide personalized treatment approaches, including targeted dietary interventions and probiotic therapies.
- Long-Term Mental Health Outcomes: Maintaining a diverse microbiome through diet, lifestyle changes, and possibly supplementation could play a protective role against the development of psychiatric disorders.
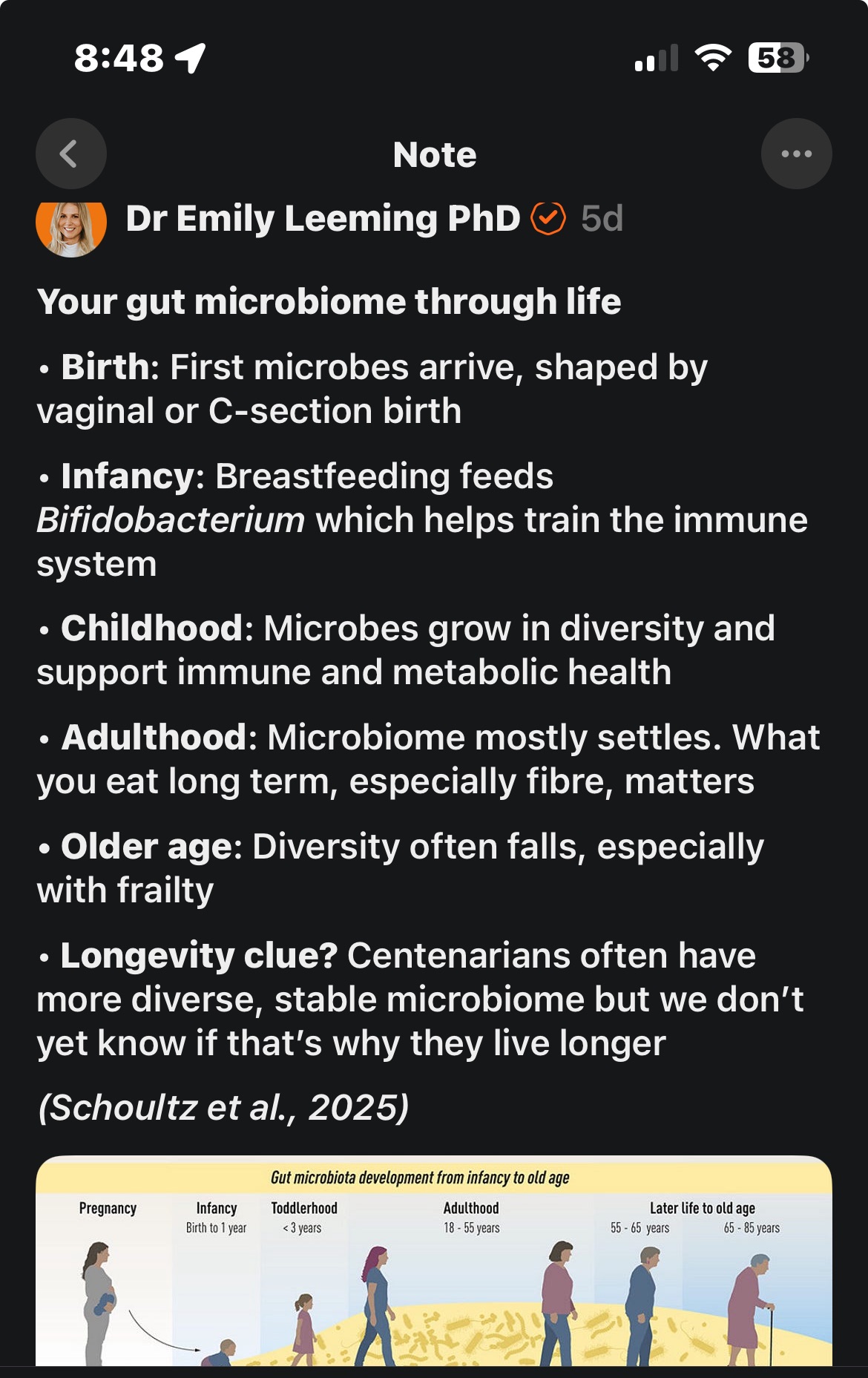
Role of Bacterial “Old Friends” in Immune System Training
Bacterial “old friends” refers to long-standing symbiotic microorganisms that have co-evolved with humans. Their role in the infant immune system includes:
- Immune Tolerance: Early exposure to these microorganisms helps in the development of immune tolerance, reducing the risk of allergic and autoimmune disorders.
- Training the Immune System: They play a crucial role in training the infant immune system, ensuring that it learns to differentiate between harmful and benign stimuli, which is vital for long-term health.
- Microbial Memory: The presence of these beneficial bacteria can create a “memory” that shapes immune responses throughout life, potentially influencing mental health outcomes.
Assessment and Treatment Planning with New Patients
When assessing and planning treatment for new patients, it is crucial to consider the gut-brain connection:
- Comprehensive Evaluation: Include questions about gastrointestinal health, diet, and any symptoms related to gut dysfunction during the initial assessment.
- Collaborative Treatment: Consider integrating dietary recommendations, probiotics, and prebiotics into treatment plans for patients presenting with mood disorders, anxiety, or related symptoms.
- Monitoring and Adjustment: Continuously monitor patients’ mental health and gut health throughout treatment to adjust protocols as needed.
Specific Minerals and Their Role
Certain minerals play a role in gut health and mental well-being:
- Zinc: Crucial for immune function, zinc levels have been linked with anxiety and depression. Supplementation may help improve mood and cognitive function.
- Magnesium: Involved in over 300 biochemical reactions, magnesium supports neurotransmitter function and may alleviate anxiety and stress.
- Iron: Essential for oxygen transport and energy production, iron deficiency can lead to fatigue and mood disturbances. Monitoring levels is critical, especially in populations prone to deficiency.
Conclusion
The intricate connection between gut health and mental well-being underscores the importance of considering the gut microbiome in psychiatric treatment. Probiotic and prebiotic interventions, along with a focus on microbiome diversity and mineral supplementation, can provide valuable support in improving mental health outcomes. Integrating this knowledge into patient assessments and treatment planning is essential for holistic mental health care.